Published March, 2023
Co-authored by Theodore R Belfor, DDS, FPFA, FIADFE; David E. McCarty, MD, FAASM and Scott Holyoak, DDS
Chronic Rhinosinusitis (CRS) is an inflammation of the paranasal sinuses lasting longer than 12 weeks and accompanied by pathologic symptoms, such as difficulty breathing, nasal congestion, and facial pain/pressure. Symptoms of nasal obstruction, nasal discharge, and hyposmia or anosmia become more prominent when CRS is complicated by nasal polyposis (NP).1
NP complicates a quarter to a third of CRS (CRS-NP) cases and occurs at a prevalence of 1-4% of the general population, with burdensome symptoms that significantly impact health-related quality of life (HRQOL).2 Moreover, CRS-NP is typically challenging to manage, with no agreed-upon pathways for a medical or surgical cure, even when the specified threshold for “success” is low.3,4 Adverse effects from medical treatments are common.
Postsurgical recurrence of polyposis is the norm. All told, CRS-NP results in a heavy burden on the healthcare system, with a high cost in lost productivity and health-related quality of life for those who suffer from it. Clearly, novel effective treatment strategies are needed.
Morphogenic Functional Appliance Therapy (MFAT) is a new practically-developed strategy that uses specialized removable oral appliances fitted with attachments that deliver intermittent signalling to the periodontal ligament, cranial bones, and cranial sutures resulting from regular movements of the tongue and contact with the appliance when swallowing. MFAT also incorporates bite blocks to increase potential space for tongue motion and, in practice, is strategically coupled with tongue mobilization and airway rehabilitation exercises5. In addition, unlike orthodontic therapy, which only moves teeth in relationship to one another, MFAT delivers dynamic messages to the cranial bones, allowing activation of dormant genetic craniofacial growth potential6.
Published studies involving this technique are few. Early reports on a predecessor for MFAT – orthotropic therapy – showed some promise in restoring palatal symmetry.7-8 However, the more widespread effects of MFAT in its current form remain anecdotal. Recently, MFAT was shown to remediate a right side-bending craniofacial dystrophy after 24 months of treatment, restoring cosmetic facial symmetry and normalizing the mandibular position (manuscript in review).
This report documents a case of a female patient who experienced a complete resolution of clinical and radiographic evidence of chronic medicallyand surgically-refractory CRS-NP following treatment with MFAT specifically targeted to expand the bony confines of the maxillary sinuses.
Report Of Case
The patient was a woman in her mid-sixties, presenting with a chief complaint of difficulty breathing through her nose within the context of a multi-year history of chronic sinus infections and complaints about sleep.
A year before her presentation, the patient presented to a board-certified otolaryngologist with complaints of persistent nasal congestion, sinus pressure, and difficulty sleeping. CBCT then demonstrated bilateral maxillary sinusitis with polyposis. (Fig. 1) The patient underwent a two-month trial of medical therapy, including inhaled corticosteroids, multiple rounds of antibiotics, and sinus irrigations, which resulted in no improvement of her symptoms. Next, she underwent sinus surgery, with bilateral 72 middle meatal antrostomy, total bilateral ethmoidectomy, bilateral frontal sinusotomy, and 73 septoplasties, which improved her nasal congestion and difficulty sleeping. However, despite these mild improvements, the patient continued to experience daily difficulty breathing through her nose and sinus pressure.
Upon presentation, 12 months after her surgery, cone-beam computed tomography (CBCT) scanning demonstrated mild improvement in the left-sided infiltrate but no change to the near-complete opacification of the right maxillary sinus, with obstruction of the ostia on that side. (Fig. 1B)


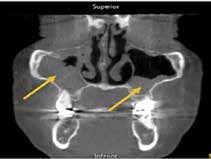

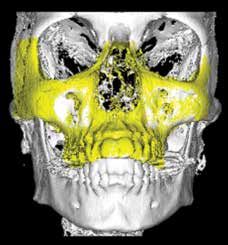
1. Coronal-view CBCT scans. A: Prior to medical therapy and otolaryngology surgery: dense bilateral maxillary sinus infiltrates are seen (yellow arrows). At surgery, polypoid tissue, pus, and granulation tissue were confirmed, confirming CRS-NP. B: 12 months after surgery, there is some improvement in the left maxillary infiltrate, but the dense infiltrate in the right maxillary sinus remains (orange arrows). 2. Coronal-view CBCT scans. A: 12 months after surgery (before MFAT) there is some improvement in the left maxillary infiltrate, but the dense infiltrate in the right maxillary sinus remains (orange arrows). B: at 4 year follow up, there is complete resolution of the maxillary infiltrates. The patient reported complete resolution of symptoms by 3 months. 3. Yellow shows midface volume increase = 13983/68 mm3 Mean = 468.24
Methods
We obtained frontal facial photos, intraoral photos, CBCT scan, and entire upper and lower dental impressions before and at treatment conclusion. MFAT consisted of an upper HomeoblockTM appliance. This device consists of Adams clasps on the bicuspids, a base plate incorporating a palatal expansion jack screw, and flap springs resting on the anterior teeth and bicuspids. A Hawley archwire extends from canine to canine. For this case, a bite block (Unilateral BiteBlock TechnologyTM) was placed on the first molar and the second bicuspid. Then we instructed the patient to wear the device during sleep and to advance the expansion screw 1-2 full turns monthly for 24 months.
The patient was lost to follow-up during 2019-2021, during the COVID-19 pandemic. She returned for follow-up after having used the MFAT appliance during sleep for four years, reporting high satisfaction with her progress.
She reported that her nasal congestion began to improve within months of initiating treatment and had entirely resolved by one year. Furthermore, she conveyed being symptom-free (nasal congestion/ facial pressure.) In addition, we obtained post-treatment CBCT scans at her (delayed) follow-up appointment, demonstrating complete resolution of maxillary infiltrates. (Fig. 2B)
At follow-up, the patient reported high satisfaction with her treatment, with complete resolution of her complaint of difficulty breathing through her nose. In addition, CBCT demonstrated complete resolution of maxillary sinus infiltrate and restoration of normal sinus architecture with patency of the maxillary ostia. (Fig. 2B)
A trained analyst/technician evaluated the pre-treatment and post-treatment CBCT scans using Analyze 14.0 software (Biomedical Imaging Resource, Mayo Clinic, MN, USA)9. Scans were first co-registered and transformed using a rigid mutual information maximization algorithm (Mayo Clinic, Rochester, MN, USA).
Next, we evaluated the images using Analyze software using an Adaptive Deformation algorithm10 to isolate the skeletal structure and calculated Preand Post-bone volumes to evaluate prepost dentoskeletal differences. Adaptive Deformation analysis demonstrated bony volume changes in the midface. (Fig. 3) Mid-face volume increased by 13,873.68 mm3.
Discussion
Re-establishing functional airflow communication between the maxillary sinuses and the nasopharynx is crucial for successfully managing CRS-NP2. In addition, increasing scientific evidence points to natural nasal nitric oxide production – and its successful ability to waft through the nasal/sinus spaces – as an essential first defence against infection.11
Surgical approaches – which necessarily involve trauma and subsequent inflammation – routinely return disappointing results, with gains achieved being short-lived and recurrence of functional blockage of the sinus ostia being commonplace.4 Medical management targeting tissue inflammation (inhaled corticosteroids, biologic agents) also routinely produce only partial responses and is frequently associated with adverse medication effects.2
This case documents the first reported successful cure of CRS-NP with a novel removable dental device (MFAT). The functional process involves remediating a subtle form of maxillary hypoplasia. MFAT physically promoted a complete expansion of the maxillary sinus, allowing the better function of the ostia, ultimately resulting in lasting functional drainage and full and durable resolution of CRS-NP.
Conclusions
MFAT is a novel and efficacious strategy for addressing bony limitations of functional airflow within the craniofacial respiratory complex. Patients suffering from CRS-NP with predominantly bony limitations to functional maxillary sinus ostia may also benefit from this technique, particularly if their disease has been refractory to usual medical and surgical treatments.

Dr. Theodore R. Belfor is a Senior Certified Instructor for the International Association for Orthodontics (IAO). He specializes in patient treatment for face and airway development in adults. His work is devoted to understanding the causes of sleep and breathing disorders through individual patient craniofacial analysis. He can be reached at drtheodorebelfor.com.
Dr. David E McCarty is a Sleep Medicine clinician, author, cartoonist, and podcast creator/host. He is the co-author of Empowered Sleep Apnea: A Handbook for Patients and the People Who Care About Them, and the creator and co-host of Empowered Sleep Apnea: THE PODCAST.
Dr. Scott Holyoak graduated in 2004 from The University of the Pacific School of Dentistry. He is the owner of Holyoak Dental in Encinitas, California. His practice is considered one of the top family and cosmetic offices in the area and treats craniofacial development and breathing issues alongside with Dr Belfor.
- Chen S, Zhou A, Emmanuel B, Thomas K, Guiang H. Systematic literature review of the epidemiology and clinical burden of chronic rhinosinusitis with nasal polyposis, Current Medical Research and Opinion, 2020. 36:11, 1897-1911, DOI: 10.1080/03007995.2020.1815682.
- Bachert c, Bhattacharyya N, Desrosiers M, Khan AH. Burden of disease in Chronic Rhinosinusitis with nasal polyps. J Asthma Allergy 2021 Feb 11;14:127-134
- Wu D, Bleier BS, Wei Y. Temporary olfactory improvement in chronic rhinosinusitis with nasal polyps after treatment. Eur Arch Otorhinolaryngol. 2018 Sep; 275(9):2193-2022. Doi: 10.1007/s00405-018-5066-5. Epub 2018 Jul 19.
- DeConde AS, Mace JC, Levy JM, Rudmik L, Alt JA, Smith TL. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope. 2017 Mar;127(3):550- 555. doi: 10.1002/lary.26391. Epub 2016 Nov 12. PMID: 27859303; PMCID: PMC5321782.
- Guimaraes KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med 2009; 179:962–966.
- Belfor TR. Epigenetic Orthodontics: Face and Airway development. Ny State Dent J 2010 Nov;(6) 18-21
- Singh GD, Diaz J, Busquets-Vaello C, Belfor TR. Facial changes following treatment with a removable orthodontic appliance in adults. Funct Orthod. 2004 Jul-Sep;21(3): 18-20, 22-3
- Belfor TR, Singh GD. Developing dental arch symmetry using the Homeoblock device. Int J Orthod 2004 15 (3): 27-30
- Robb RA, Hanson DP. “ANALYZE: A software system for biomedical image analysis” In Proceedings of the First Conference on Visualization in Biomedical Computing, IEEE publications, New York, NY, 1990
- Algorri M, Schmitt F. “Reconstructing the Surface of Unstructured 3D Data,” SPIE Proceedings Vol 2431, Medical Imaging 1995: Image Display
- Lundberg JO. Nitric oxide and the paranasal sinuses. Anat Rec (Hoboken). 2008 Nov;291(11):1479-84. doi: 10.1002/ar.20782. PMID: 18951492.