Introduction
The American Association of Orthodontists White Paper: Obstructive Sleep Apnea and Orthodontics states, under the term “Etiology,” “Obstructive Sleep Apnea occurs as a function of increased collapsibility of the upper airway. The pharyngeal critical closing pressure (Pcrit) is the pressure at which the upper airway collapses. This collapsibility is influenced further by impaired neuromuscular tone.”1 Comparing the size and shape of the pharyngeal airway for Obstructive Sleep Apnea (OSA) patients and non-OSA patients, research shows that the minimum cross-sectional area (min. area) and anterior-posterior (AP) dimension exhibit significant differences. Statistically, the AP dimension and the min. area of the OSA group are significantly smaller than those of the non-OSA group.2,3 These studies confirm that the AP dimension of the airway and the cross-sectional area of the narrowest airway slice in the oropharynx are significantly smaller in OSA patients compared to non-OSA subjects. It is the purpose of this article to demonstrate, through multiple case studies, that dental appliance therapy increases the pharyngeal airway size and shape, which may be related to improved airway tone and reduced collapsibility.
Methods
A cone beam computerized tomographic (CBCT) scan was taken of the patient before treatment and again after 12 or 24 months. Upper and lower dental models were made and Homeoblock™ dental appliances were fabricated for the patient.4,5,6 The Homeo-block utilizes an orthodontic expansion screw along with Unilateral Bite Block Technology™. The unilateral 5mm bite block is placed on the second bicuspid and first molar on the less developed side of the face, which is the side that can have a deeper nasolabial depression or lower eye, thinner upper lip, or deeper pre-jowl region. The appliances were worn a maximum of 12 hours each day (mainly during sleep) for up to 24 months. The patient was instructed to advance the expansion screw 0.125 mm (1/4 turn) each week. The patient returned periodically for minor adjustments.
Independent evaluation of the pre- and post-treatment CBCT scans was performed by an analysis technician using Analyze 14.0 software (Biomedical Imaging Resource, Mayo Clinic, MN, USA) to obtain airway volume and minimum cross-sectional area measurements. Pre- and post-treatment scans were first co-registered and transformed using a rigid mutual information maximization algorithm. Next, the pre-treatment and transformed post-treatment scans were used as an input for segmentation. Upper airway segmentation was achieved by setting limits using morphological landmarks common to both input volumes; the epiglottis as a lower limit and the palatine bone as the upper limit. A 3D region-growing algorithm was then utilized to isolate the pre-treatment and post-treatment airways. The resulting airway volumes and axial cross-sectional areas at the narrowest point in the pre-treatment and corresponding location in the post-treatment airway were calculated.
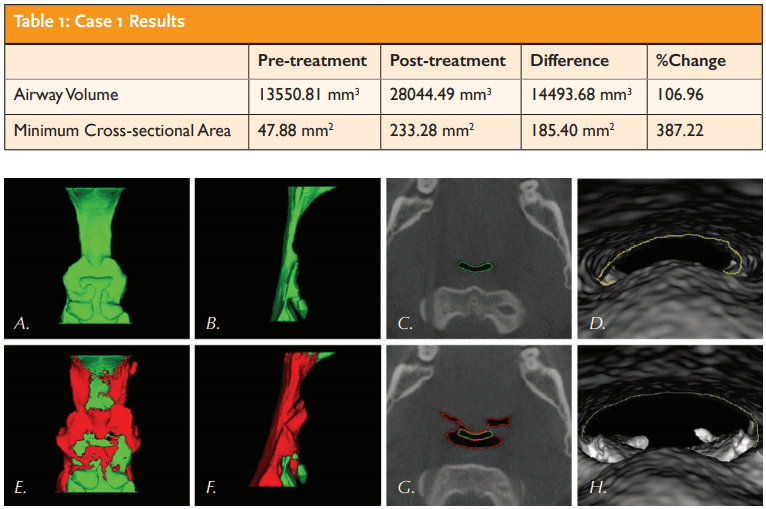
Case Study 1
Background: A 35-year-old male with moderate sleep apnea, was referred by a board-certified sleep physician as he did not want to wear a CPAP.
Results: Table 1 and Figure 1.
Outcome: Treatment decreased the patient’s Apnea Hypopnea Index from 27 to 5. The patient is no longer required to wear a CPAP.
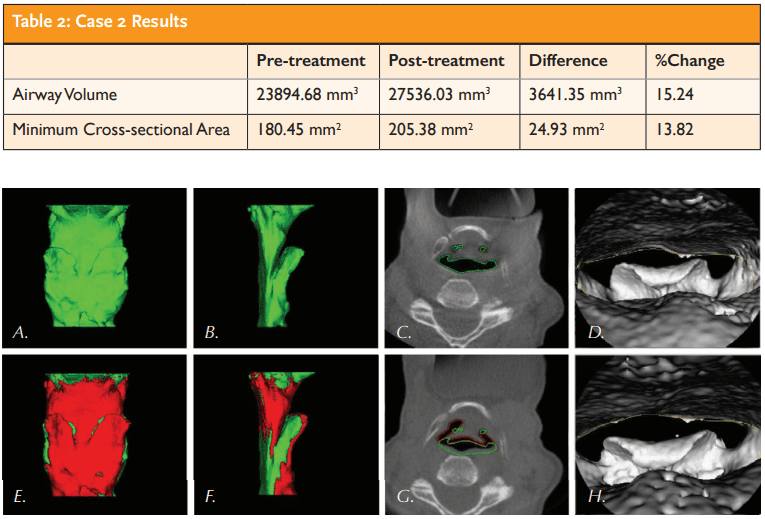
Case Study 2
Background: A 72-year-old patient presented with the complaint of being tired in the morning.
Results: Table 2 and Figure 2.
Outcome: Post-treatment the patient states, “I am able to bring my jaw forward, and my breathing has become deeper. I feel so much better.”
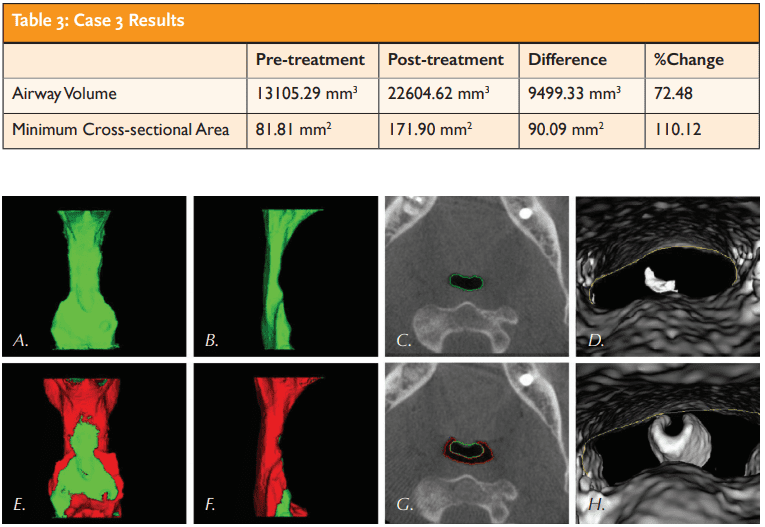
Case Study 3
Background: A 58-year-old male was treated after reporting problems sleeping due to snoring, headaches, and overall body pain.
Results: Table 3 and Figure 3.
Outcome: After treatment the patient reports, “I feel so much better, no more headaches.”
Discussion
The collapse of the pharyngeal airway during sleep has serious health consequences such as disrupted sleep, reduce oxygen saturation levels, and OSA. The physiological mechanism causing such conditions is closely related to flow in tubes. Airflow modeling in Starling resistors has revealed a variety of dynamics involved in compressed collapsible tube systems such as our airway.7 The base of the tongue represents the “bottleneck” region in the human airway, and constriction in this region can have adverse effects both upstream and downstream from this point.
Both inspiratory and expiratory flow limitations can be created by a lack of space at the base of the tongue. Turbulent airflow increases tongue collapsibility, further exasperating the problem and a smaller, less toned muscular airway reduces airway volume with a decrease in patient’s Pcrit, increasing the number of apneic events.8
The presented timeline case studies demonstrate that it may be possible to remodel the muscular tube, which is the pharyngeal airway. Both the pre-treatment and post-treatment images were obtained without the appliance in place. The increases in airway volume were also measured and calculated without the appliance in place. The traditional treatments for OSA (CPAP and Mandibular Advancement Devices) serve to open the airway only while being worn and have not yet demonstrated increased airway volume while not utilizing the devices. Although these treatments are intended for nocturnal use, the presented data demonstrate anatomical improvements while awake, when not wearing the appliance.
The case studies show an increase in volume, especially in the area posterior to the tongue and in the region bounded by the back and side walls of the throat. The increase in airway volume provides greater airflow and reduces the “bottleneck” – the main source of turbulence and resistance behind the tongue.
We hypothesize that the measurable increases in airway volume are obtained in several ways, due to the design of the oral appliance. 1) By altering swallowing patterns while wearing the appliance, it acts as a tongue trainer. The appliance provides a platform that engages the tongue near the roof of the mouth when swallowing. It is postulated this action eventually retrains the tongue during waking hours while toning the muscles at the base of the tongue. This myofunctional therapy occurs every night while the patient sleeps and helps to tone the muscles that raise the tongue, such as the stylohyoid, mylohyoid muscles, genioglossus, and hyoglossus muscles. Furthermore, the pharyngeal constrictor muscles that comprise the airway have been toned by the actions of the lips and cheeks while wearing the appliance. 2) The design of the appliance helps the obicularis oris and buccinator to function in a way that may help stimulate the superior pharyngeal constrictor and help tone the muscle. The buccinator is joined to the superior pharyngeal constrictor by the pterygomandibular raphe, and light stimulation of these muscles may help provide the toning evident in the presented data.
Conclusion
The results that we see here can be related to the simple concept that form follows function. By improving the function of swallowing by toning the muscles while sleeping, we can improve the form of the pharyngeal airway while awake.
Dentists may play an important role in the detection of OSA in patients through careful oropharyngeal examination in routine dental treatment. It is postulated that this treatment can reduce or delay the onset of OSA in some individuals and needs to be studied in controlled clinical trials.
Theodore R. Belfor, DDS, is a graduate of New York University College of Dentistry, a Senior Certified Instructor for the International Association for Orthodontics (IAO) and has been in private practice for more than 40 years. Since 2001, Dr. Belfor has specialized in patient treatment with the Homeoblock™ orthopedic/orthodontic appliance designed with the Unilateral Bite Block technology®, for face and airway development in adults. Dr. Belfor has been lecturing, teaching and training dentists with the Homeoblock™ and his unique diagnostic protocol for more than 18 years worldwide. His work is devoted to understanding the causes of sleep and breathing disorders through individual patient craniofacial analysis. Dr. Belfor has been published in numerous journals. He can be reached through his site at drtheodorebelfor.com.
Michael Philcock is a product manager for AnalyzeDirect. He has more than 15 years of experience in the processing and analysis of biomedical imaging data for a wide range of biological applications in the healthcare, life sciences, pharmaceutical, and biotech industries.
Scott Simonetti, DDS, earned his Bachelor of Science in Nutritional Sciences from Cornell University and then attended the University at Buffalo School of Dental Medicine where he earned his DDS degree. Dr. Simonetti has been in private general practice on Long Island since 2001. He is the inventor of the FDA cleared and patented custom oral orthotic, The POD®. Dr. Simonetti has lectured at multiple continuing education programs and has appeared on national radio programs and blogs, discussing stem cells, nitric oxide, mitochondria, intermittent hypoxia and disordered breathing. He is the Co-Founder and CEO of Advanced Facialdontics LLC, a company that designs and develops novel oral orthotics. He has presented research to the Department of Defense at the Military System Health Research Symposium in Kissimmee, Florida and has a passion to help military personnel and first responders.
- American Association of Orthodontists White Paper: Obstructive Sleep Apnea and Orthodontics
- Barrera E J, Pau CY, Forest VI et al. Anatomic measures of upper airway structures in obstructive sleep apnea. World Journal of Otorhinolaryngology Head and Neck Surg. 2017 Jun; 3(2): 85–91.
- Svaza J, Skagers A, Cakarne D, Upper airway sagittal dimensions in obstructive apnea (OSA) patients and severity of the disease. Stomatology. 2011;13 (4):123-7
- Belfor, TR Epigenetic orthodontics. Face and airway development vol. 18. NYSDJ Nov 2010
- Belfor TR, Singh GD Developing dental symmetry using an intraoral device. A case report JCD vol. 20 (2) 2004
- Belfor TR, Mahony D Improving the adult dental arch, and airway, through bioengineering and dentofacial orthopedics. Aest Dent Today vol. 5 (3) May 2011
- Bertram CD, Raymond CJ, Pedley TJ. Application of nonlinear dynamics concepts to the analysis of self-excited oscillations of a collapsible tube conveying a fluid. Journal of Fluids and Structures, vol. 5, no.4, pp. 391-426, 1991.
- Rasani MR, Inthavong K, Tu JY. Simulation of pharyngeal airway Interaction with air flow using a low-Re turbulence model. Modeling and Simulation in Engineering. volume 2011